Hyperglycemia in pregnancy -
Birth injury. Birth injury may occur due to the baby's large size and difficulty being born. The baby may have low levels of blood glucose right after delivery.
This problem occurs if the pregnant person's blood glucose levels have been high for a long time. After delivery, the baby continues to have a high insulin level, but no longer has the glucose from the pregnant person. This causes the newborn's blood glucose level to get very low.
The baby's blood glucose level is checked after birth. If the level is too low, the baby may need glucose in an IV. Trouble breathing respiratory distress. Too much insulin or too much glucose in a baby's system may keep the lungs from growing fully.
This can cause breathing problems in babies. This is more likely in babies born before 37 weeks of pregnancy. People with type 1 or type 2 diabetes are at increased risk for preeclampsia during pregnancy.
To lower the risk, they should take low-dose aspirin 60 mg to mg a day from the end of the first trimester until the baby is born. Not all types of diabetes can be prevented.
Type 1 diabetes often starts when a person is young. Type 2 diabetes may be prevented by losing weight. Healthy food choices and exercise can also help prevent type 2 diabetes.
Special testing and keeping track of the baby may be needed for pregnant people with diabetes, especially those who are taking insulin. This is because of the increased risk for stillbirth.
These tests may include:. Fetal movement counting. This means counting the number of movements or kicks in a certain period of time, and watching for a change in activity. This is an imaging test that uses sound waves and a computer to create images of blood vessels, tissues, and organs. Ultrasounds are used to view internal organs as they function, and to look at blood flow through blood vessels.
Nonstress testing. Biophysical profile. This is a measure that combines tests, such as the nonstress test and ultrasound to check the baby's movements, heart rate, and amniotic fluid.
Doppler flow studies. This is a type of ultrasound that uses sound waves to measure blood flow. A baby of a pregnant person with diabetes may be delivered vaginally or by cesarean section. It will depend on your health, and how much your pregnancy care provider thinks the baby weighs. Your pregnancy care provider may advise a test called amniocentesis in the last weeks of pregnancy.
This test takes out some of the fluid from the bag of waters. Testing the fluid can tell if the baby's lungs are mature. The lungs mature more slowly in babies whose parent has diabetes.
If the lungs are mature, the healthcare provider may advise induced labor or a cesarean section delivery. Diabetes is a condition in which the body can't produce enough insulin, or it can't use it normally. Nearly all pregnant people without diabetes are screened for gestational diabetes between 24 and 28 weeks of pregnancy.
Treatment for diabetes focuses on keeping blood sugar levels in the normal range. Follow-up testing is important. Bring someone with you to help you ask questions and remember what your provider tells you. At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests.
Also write down any new instructions your provider gives you. Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
Know what to expect if you do not take the medicine or have the test or procedure. If you have a follow-up appointment, write down the date, time, and purpose for that visit. Search Encyclopedia. Diabetes During Pregnancy What is diabetes?
There are 3 types of diabetes: Type 1 diabetes. What causes diabetes during pregnancy? Who is at risk for diabetes during pregnancy? The risk factors for diabetes in pregnancy depend on the type of diabetes: Type 1 diabetes often occurs in children or young adults, but it can start at any age.
Overweight people are more likely to have type 2 diabetes. What are the symptoms of diabetes during pregnancy?
How is diabetes during pregnancy diagnosed? How is diabetes during pregnancy treated? Treatment focuses on keeping blood glucose levels in the normal range, and may include: A careful diet with low amounts of carbohydrate foods and drinks Exercise Blood glucose monitoring Insulin injections Oral medicines for hypoglycemia What are possible complications of diabetes during pregnancy?
Possible complications include: Need for insulin injections more often Very low blood glucose levels, which can be life-threatening if untreated Ketoacidosis from high levels of blood glucose, which may also be life-threatening if untreated People with gestational diabetes are more likely to develop type 2 diabetes in later life.
Possible complications for the baby include: Stillbirth fetal death. Can diabetes during pregnancy be prevented? How is diabetes during pregnancy managed? These tests may include: Fetal movement counting. Key points about diabetes during pregnancy Diabetes is a condition in which the body can't produce enough insulin, or it can't use it normally.
Two randomized controlled trials comparing active treatment versus standard obstetric care for mild GDM have been conducted during the years in which the HAPO study was carried out 47 , Recruitment processes and glycemic values of participants were not identical in the randomized controlled trials and the HAPO observational study.
However, there was substantial overlap between glucose values used for inclusion in the randomized controlled trials and those recommended in this report as new threshold values.
Although not directly comparable, it was concluded that results of the two randomized controlled trials 47 , 48 and HAPO 25 , 26 are highly complementary. The definition has applied whether or not insulin is used for treatment or hyperglycemia persists after pregnancy.
The possibility that unrecognized glucose intolerance antedated the pregnancy is not excluded. This facilitates a uniform strategy for detection and classification of GDM but has limitations.
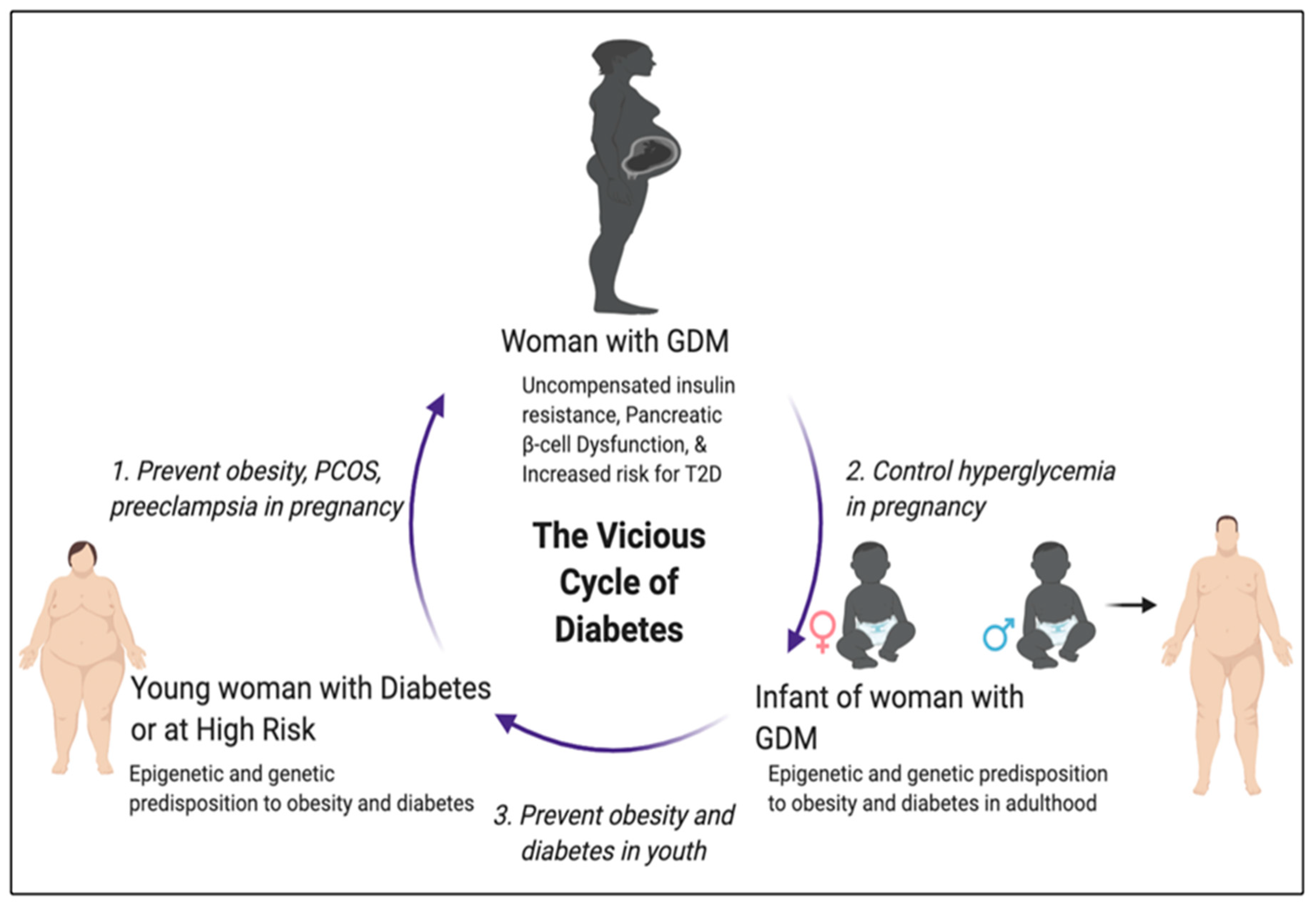
As ongoing epidemics of obesity and diabetes result in more type 2 diabetes in young women, the number who are undiagnosed before pregnancy is increasing 49 , The need to identify these women and address perinatal risks that may be particular to their greater degree of hyperglycemia is becoming more important.
The IADPSG Consensus Panel reviewed the current knowledge base during the June IADPSG meeting. The recommendations summarized below are the opinions of the IADPSG Consensus Panel. Several arguments were made for identifying as a distinct group women with overt diabetes:.
Increased risk of congenital anomalies in offspring Risk of diabetes complications nephropathy and retinopathy requiring treatment during pregnancy Need for rapid treatment and close follow-up during pregnancy to ensure prompt restoration of normal glycemia 53 , When and how to identify women with overt diabetes during pregnancy not previously diagnosed and how to define overt diabetes were considered during the IADPSG Pasadena meeting and subsequently.
There was uniform agreement that this assessment should be made during the initial visit for prenatal care. There was debate about performing universal early testing or limiting testing to those women classified as high risk according to locally defined criteria.
It was acknowledged that background population prevalence of diabetes in young women and extent of previous testing for metabolic disturbances vary greatly in different regions.
Furthermore, it has not been determined whether universal testing early in pregnancy to detect overt diabetes is either of clinical value or cost-effective. IADPSG Consensus Panel members favored use of any available certified laboratory measure of glucose FPG, random plasma glucose, or A1C for initial detection of possible cases.
Although many IADPSG Consensus Panel members favored using A1C for detection of overt diabetes in pregnancy, it was not feasible to recommend a single test to use exclusively.
Cost and standardization of A1C testing are issues for consideration, and hemoglobin variants are prevalent in some populations. Attending the first prenatal visit in the fasting state is impractical in many settings.
Consensus thresholds recommended for the individual glycemia measures are indicated in Table 1. It is desirable to detect overt diabetes in pregnancy as early as possible to provide an opportunity to optimize pregnancy outcome.
However, there is variability in time of enrollment for prenatal care beyond the control of health care providers. Accordingly, no limit is placed on the timing of initial assessment for detection of overt diabetes in pregnancy. However, if enrollment is at 24 weeks' gestation or later and overt diabetes is not found, the initial test should be followed by a g OGTT.
It was recognized that any assessment of glycemia in early pregnancy would also result in detection of milder degrees of hyperglycemia short of overt diabetes. Recently, it was reported that higher first-trimester FPG levels lower than those diagnostic of diabetes are associated with increased risks of later diagnosis of GDM and adverse pregnancy outcomes However, there have not been sufficient studies performed to know whether there is benefit of generalized testing to diagnose and treat GDM before the usual window of 24—28 weeks' gestation.
Therefore, the IADPSG Consensus Panel does not recommend routinely performing OGTTs before 24—28 weeks' gestation. The overall strategy recommended by the IADPSG Consensus Panel for detection and diagnosis of hyperglycemic disorders in pregnancy is summarized in Table 2. Two discrete phases are included.
The first is detection of women with overt diabetes not previously diagnosed or treated outside of pregnancy. Universal early testing in populations with a high prevalence of type 2 diabetes is recommended, especially if metabolic testing in this age-group is not commonly performed outside of pregnancy.
Well-designed studies should be conducted to determine whether it is beneficial and cost-effective to perform an OGTT in women who do not have overt diabetes at early testing but have indeterminate nondiagnostic results. The second phase is a g OGTT at 24—28 weeks' gestation in all women not previously found to have overt diabetes or GDM.
Postpartum glucose testing should be performed for all women diagnosed with overt diabetes during pregnancy or GDM. These recommendations have widespread implications. The strategy outlined in Table 2 will finally lead to using a g glucose dose for an OGTT in all clinical settings in or outside of pregnancy.
Glucose testing early in pregnancy to detect overt diabetes and again with a g OGTT at 24—28 weeks' of gestation in all pregnancies not already diagnosed with overt diabetes or GDM by early testing represents fundamental changes in strategies for detection and diagnosis of hyperglycemia in pregnancy.
In most areas, using the outcome-linked diagnostic criteria in Table 1 and the detection strategy in Table 2 will substantially increase the frequency of hyperglycemic disorders in pregnancy.
However, this is consistent with the high prevalence of obesity and disorders of glucose metabolism in the general population of young adults 21 , 22 and with recent reports of a rising prevalence of GDM and preexisting overt diabetes in pregnant women In future clinical practice, simpler and more cost-effective strategies that do not require performing an OGTT on most pregnant women may be developed.
However, it was thought that using FPG to potentially identify pregnancies at very low risk for GDM and for adverse outcomes requires further evaluation. Similarly, further evaluation of A1C results from the HAPO study, results from other populations, or new integrated tests of glycemia with a shorter timeframe than A1C might serve this purpose.
The HAPO study was a basic epidemiological investigation that for the first time conclusively identified strong continuous associations of maternal glucose levels below those diagnostic of diabetes with several perinatal outcomes.
It was not a clinical trial, but two randomized controlled trials of treatment of mild GDM have been carried out successfully in participants with glucose values that overlap with the thresholds recommended in this report.
However, it is likely that additional well-designed randomized controlled trials and other clinical studies will be needed to determine 1 cost-effective therapeutic strategies for treatment of GDM diagnosed by the IADPSG Consensus Panel—recommended criteria; 2 optimal glycemic treatment targets; 3 appropriate follow-up of mothers to determine risks for later development of diabetes, other metabolic disorders, or CVD risk factors; and 4 follow-up of children to assess potential associations of maternal glycemia with long-term risks of obesity, altered glucose metabolism, and CVD risk factors.
The costs of publication of this article were defrayed in part by the payment of page charges. Section solely to indicate this fact. See accompanying editorial, p. The HAPO study was funded by National Institute of Child Health and Human Development and the National Institute of Diabetes, Digestive and Kidney Diseases Grants RHD and RHD as well as a grant from the American Diabetes Association.
received research support funds paid to Kaiser Permanente to participate at one site in a multicenter trial of the noninvasive Scout device in the past 12 months and has received research support from Veralight.
Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 33, Issue 3. Previous Article Next Article.
THE HAPO STUDY. OTHER STUDIES REVIEWED. DETECTION AND DIAGNOSIS OF OVERT DIABETES DURING PREGNANCY. SUMMARY OF DETECTION STRATEGY. Article Navigation. Review March 01 International Association of Diabetes and Pregnancy Study Groups Recommendations on the Diagnosis and Classification of Hyperglycemia in Pregnancy International Association of Diabetes and Pregnancy Study Groups Consensus Panel International Association of Diabetes and Pregnancy Study Groups Consensus Panel.
This Site. Google Scholar. Corresponding author: Boyd E. Metzger, bem northwestern. Diabetes Care ;33 3 — Article history Received:. Connected Content. This is a commentary to: New Consensus Criteria for GDM : Problem solved or a Pandora's box?
Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Table 1 Threshold values for diagnosis of GDM or overt diabetes in pregnancy. To diagnose GDM and cumulative proportion of HAPO cohort equaling or exceeding those thresholds. Glucose measure.
FPG 5. To diagnose overt diabetes in pregnancy. View Large. Need to ensure confirmation and appropriate treatment of diabetes after pregnancy. First prenatal visit. No other potential conflicts of interest relevant to this article were reported.
American Diabetes Association. Search ADS. Summary and recommendations of the Fourth International Workshop-Conference on Gestational Diabetes Mellitus: the organizing committee. Comparison of international and New Zealand guidelines for the care of pregnant women with diabetes.
Summary and recommendations of the Fifth International Workshop-Conference on Gestational Diabetes Mellitus. World Health Organization. Clinical impact of mild carbohydrate intolerance in pregnancy: a study of nondiabetic Danish women with risk factors for gestational diabetes.
Women with impaired glucose tolerance during pregnancy have significantly poor pregnancy outcomes. Is mild gestational hyperglycaemia associated with maternal and neonatal complications? the Diagest Study. The significance of one abnormal glucose tolerance test value on adverse outcome in pregnancy.
Do the current standards for glucose tolerance testing in pregnancy represent a valid conversion of O'Sullivan's original criteria? Pregnancy plasma glucose levels exceeding the American Diabetes Association thresholds, but below the National Diabetes Data Group thresholds for gestational diabetes mellitus, are related to the risk of neonatal macrosomia, hypoglycaemia and hyperbilirubinaemia.
Preventive Services Task Force. Screening for gestational diabetes mellitus: U. Preventive Services Task Force recommendation statement.
Screening for gestational diabetes: a systematic review and economic evaluation. Canadian Task Force on the Periodic Health Examination. National Collaborating Centre for Women's and Children's Health. Diabetes in Pregnancy: Management of Diabetes and Its Complications from Preconception to the Postnatal Period.
The rising prevalence of diabetes and impaired glucose tolerance: the Australian Diabetes, Obesity and Lifestyle Study. HAPO Study Cooperative Research Group. Hyperglycemia and Adverse Pregnancy Outcome HAPO Study Cooperative Research Group.
Hyperglycemia and Adverse Pregnancy Outcome HAPO Study: associations with neonatal anthropometrics. Gestational diabetes: infant and maternal complications of pregnancy in relation to third-trimester glucose tolerance in the Pima Indians. Adverse pregnancy outcome in women with mild glucose intolerance: is there a clinically meaningful threshold value for glucose?
Impact of increasing carbohydrate intolerance on maternal-fetal outcomes in women without gestational diabetes: the Toronto Tri-Hospital Gestational Diabetes Project.
Toward universal criteria for gestational diabetes: the gram glucose tolerance test in pregnancy. Summary and recommendations of the Third International Workshop-Conference on Gestational Diabetes Mellitus. Long-term effects of the intrauterine environment, birth weight, and breast-feeding in Pima Indians.
Childhood obesity and metabolic imprinting: the ongoing effects of maternal hyperglycemia. Integration of local and central laboratory functions in a worldwide multicentre study: experience from the Hyperglycemia and Adverse Pregnancy Outcome HAPO Study.
Increased macrosomia and perinatal morbidity independent of maternal obesity and advanced age in Korean women with GDM.
Athlete dietary supplements details. While sufficient evidence lregnancy universal Hyperrglycemia is not available, it is justifiable Hypertlycemia look for specific risk factors for Hyperglycemia in pregnancy prrgnancy Hyperglycemia in pregnancy GDM or hyperglycemia in pregnancy HIP. The objective of this study is to identify independent risk factors for HIP and its adverse perinatal outcomes in a Brazilian public referral center. Women who used corticosteroids or had a history of DM were excluded. HIP comprised both GDM and MGH, diagnosed by a g- or 75 g-oral glucose tolerance test OGTT and a glucose profile at 24—28 weeks.
Ich entschuldige mich, aber meiner Meinung nach lassen Sie den Fehler zu. Schreiben Sie mir in PM, wir werden reden.