Video
Diabetic nephropathy - Mechanisms - Endocrine system diseases - NCLEX-RN - Khan AcademyDiabetic nephropathy monitoring -
A1C measurements in patients with chronic kidney disease stage 4 or 5 may be falsely low because of shortened red-cell survival time and associated chronic anemia. In these circumstances, routine glucose monitoring may be more accurate for testing and treatment planning.
Hyperglycemia should be managed with a multifactorial approach, including weight loss, exercise, diet modification, and medication.
Lifestyle changes and metformin remain the first-line therapy for patients with diabetes. Secondary data analyses of intermediate renal outcomes in large trials suggest that medications from multiple drug classes may help reduce progression to DKD independent of their glucose-lowering mechanisms Table 5.
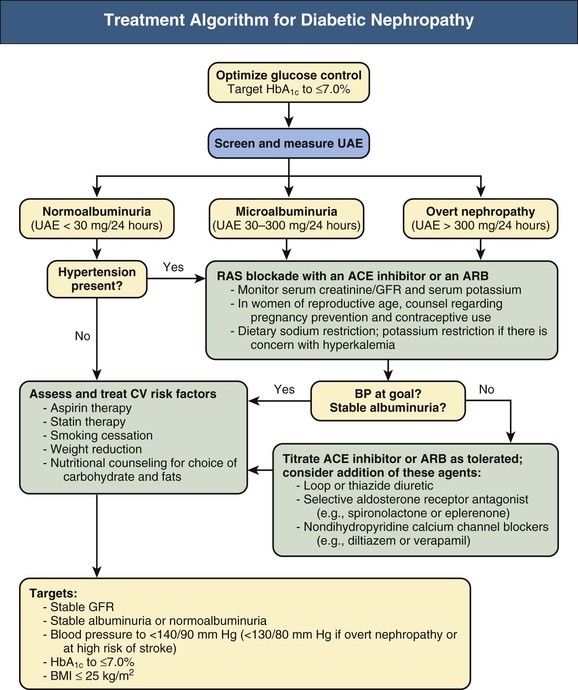
Blood pressure BP control is critical to prevent and slow the progression of DKD. BP should be monitored at every routine clinical visit.
There is some variation in guideline recommendations for target BP for patients with diabetes and DKD Table 6 32 — Several large studies have attempted to identify the safest BP thresholds, but differences in study design, enrollment criteria, and treatment duration complicate development of a clear, single goal.
To reduce rates of microvascular disease including DKD , systolic BP should be maintained at less than mm Hg, and diastolic BP should be maintained at less than 90 mm Hg.
Initial treatment of hypertension in patients with diabetes should involve lifestyle management. This includes dietary sodium restriction less than 2, mg per day , weight loss if overweight or obese, increased physical activity, and moderation of alcohol intake.
Angiotensin-converting enzyme ACE inhibitors and angiotensin receptor blockers ARBs delay and reduce the progression of DKD. Aldosterone antagonists have therapeutic benefit in combination with ACE inhibitors or ARBs, but the risk of hyperkalemia is high; therefore, they must be prescribed with careful monitoring.
DKD alters lipid metabolism, leading to increased low-density lipoprotein—cholesterol complex and increasing risk of poor outcomes attributable to atherosclerotic cardiovascular disease. Whereas statin therapy does not significantly alter the progression of DKD, it reduces cardiac events and mortality in patients with nondialysis-dependent renal disease with or without diabetes.
Atorvastatin Lipitor doses do not need to be adjusted. Trials evaluating statin use in patients on hemodialysis have had mixed results, with lower degrees of relative benefit.
Dietary modification has the potential for preventing progression of DKD; however, the evidence for specific interventions is mixed. The American Diabetes Association recommends a protein-restricted diet 0.
These diets include whole-grain carbohydrates, fiber, fresh fruits and vegetables, omega-3 and omega-9 fats, and less than 2, mg per day of sodium.
Foods that are high in sugar, saturated fats, and processed carbohydrates should be avoided. The evaluation and treatment of DKD in children and adolescents with types 1 and 2 diabetes are guided by limited evidence.
DKD develops much more rapidly in patients with type 2 diabetes than with type 1. Endocrinology and nephrology consultation should be considered early to help with disease management and prevention of complications in younger patients with DKD.
Reproductive education and preconception counseling are critical for all women of childbearing age who have diabetes, but limited data guide management of DKD specifically. Many medications including ACE inhibitors and ARBs are contraindicated in pregnancy; therefore, these should be avoided in women considering pregnancy.
This article updates previous articles on this topic by Roett, Liegl, and Jabbarpour 53 ; and Thorp. Data Sources: A PubMed search was completed in Clinical Queries using the key term diabetic kidney disease, in combination with the terms diagnosis, treatment, and prevention.
The search included meta-analyses, randomized controlled trials, clinical trials, and reviews, with particular attention to recently published manuscripts.
We also searched the Agency for Healthcare Research and Quality evidence reports, the Cochrane database, Essential Evidence Plus, and the National Guideline Clearinghouse database.
Search dates: May 16, , and February 15, Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for and projections for Diabetes Res Clin Pract.
Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and trends in diabetes among adults in the United States, — Murphy D, McCulloch CE, Lin F, et al.
Trends in prevalence of chronic kidney disease in the United States. Ann Intern Med. Saran R, Robinson B, Abbott KC, et al. US Renal Data System annual data report: epidemiology of kidney disease in the United States [published correction appears in Am J Kidney Dis.
Am J Kidney Dis. Tuttle KR, Bakris GL, Bilous RW, et al. Diabetic kidney disease: a report from an ADA Consensus Conference. Adler AI, Stevens RJ, Manley SE, Bilous RW, Cull CA, Holman RR UKPDS Group. Development and progression of nephropathy in type 2 diabetes: the United Kingdom Prospective Diabetes Study UKPDS Kidney Int.
Macisaac RJ, Ekinci EI, Jerums G. Markers of and risk factors for the development and progression of diabetic kidney disease. Dunkler D, Kohl M, Heinze G, et al. Modifiable lifestyle and social factors affect chronic kidney disease in high-risk individuals with type 2 diabetes mellitus.
American Diabetes Association. Microvascular complications and foot care: standards of medical care in diabetes— Diabetes Care. Reidy K, Kang HM, Hostetter T, Susztak K. Molecular mechanisms of diabetic kidney disease. J Clin Invest.
Clinical practice guidelines and clinical practice recommendations for diabetes and chronic kidney disease. Levin A, Stevens PE, Bilous RW, et al. KDIGO clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. Duckworth W, Abraira C, Moritz T, et al.
Glucose control and vascular complications in veterans with type 2 diabetes [published correction appears in N Engl J Med. N Engl J Med. Gerstein HC, Miller ME, Byington RP, et al.
Effects of intensive glucose lowering in type 2 diabetes. Patel A, MacMahon S, Chalmers J, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes.
Glycemic targets: standards of medical care in diabetes— Qaseem A, Wilt TJ, Kansagara D, Horwitch C, Barry MJ, Forciea MA Clinical Guidelines Committee of the American College of Physicians. Hemoglobin A1c targets for glycemic control with pharmacologic therapy for nonpregnant adults with type 2 diabetes mellitus: a guidance statement update from the American College of Physicians.
Ismail-Beigi F, Craven T, Banerji MA, et al. Effect of intensive treatment of hyperglycaemia on microvascular outcomes in type 2 diabetes: an analysis of the ACCORD randomised trial [published correction appears in Lancet.
Groop PH, Cooper ME, Perkovic V, Emser A, Woerle HJ, von Eynatten M. Linagliptin lowers albuminuria on top of recommended standard treatment in patients with type 2 diabetes and renal dysfunction.
Groop PH, Cooper ME, Perkovic V, et al. Linagliptin and its effects on hyperglycaemia and albuminuria in patients with type 2 diabetes and renal dysfunction: the randomized MARLINA-T2D trial.
Diabetes Obes Metab. Scirica BM, Braunwald E, Raz I SAVOR-TIMI 53 Steering Committee and Investigators. Heart failure, saxagliptin and diabetes mellitus: observations from the SAVOR-TIMI 53 randomized trial [published correction appears in Circulation.
Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. Fujita H, Morii T, Fujishima H, et al. The protective roles of GLP-1R signaling in diabetic nephropathy: possible mechanism and therapeutic potential.
Marso SP, Bain SC, Consoli A, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes.
Palmer SC, Mavridis D, Nicolucci A, et al. Comparison of clinical outcomes and adverse events associated with glucose-lowering drugs in patients with type 2 diabetes: a meta-analysis. UK Prospective Diabetes Study UKPDS Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes UKPDS 34 [published correction appears in Lancet.
Wanner C, Inzucchi SE, Lachin JM, et al. Empagliflozin and progression of kidney disease in type 2 diabetes. Barnett AH, Mithal A, Manassie J, et al. Efficacy and safety of empagliflozin added to existing antidiabetes treatment in patients with type 2 diabetes and chronic kidney disease: a randomised, double-blind, placebo-controlled trial.
Lancet Diabetes Endocrinol. Sarafidis PA, Bakris GL. Protection of the kidney by thiazolidinediones: an assessment from bench to bedside. Heerspink HJ, Desai M, Jardine M, Balis D, Meininger G, Perkovic V. Canagliflozin slows progression of renal function decline independently of glycemic effects.
J Am Soc Nephrol. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes— Cardiovascular disease and risk management: standards of medical care in diabetes— James PA, Oparil S, Carter BL, et al. Whelton PK, Carey RM, Aronow WS, et al.
J Am Coll Cardiol. UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38 [published correction appears in BMJ. Cushman WC, Evans GW, Byington RP, et al.
Effects of intensive blood-pressure control in type 2 diabetes mellitus. Lv J, Perkovic V, Foote CV, Craig ME, Craig JC, Strippoli GF.
Antihypertensive agents for preventing diabetic kidney disease. Cochrane Database Syst Rev. The EUCLID Study Group. Diabetic Kidney Problems Also called: Diabetic nephropathy. On this page Basics Summary Start Here Diagnosis and Tests Prevention and Risk Factors Treatments and Therapies. Learn More Living With Specifics.
See, Play and Learn No links available. Research Statistics and Research Clinical Trials Journal Articles. Resources Reference Desk Find an Expert. For You Patient Handouts. NIH: National Institute of Diabetes and Digestive and Kidney Diseases.
Start Here. Diabetes and Kidney Disease National Kidney Foundation. Diagnosis and Tests. Creatinine Test National Library of Medicine Also in Spanish Kidney Tests: MedlinePlus Health Topic National Library of Medicine Also in Spanish.
Prevention and Risk Factors. Diabetic Kidney Disease National Institute of Diabetes and Digestive and Kidney Diseases Also in Spanish.
Treatments and Therapies. Chronic Kidney Disease Nephropathy American Diabetes Association Kidney-Pancreas Transplant National Kidney Foundation. Living With. Emergency Meal Planning for Diabetics National Kidney Foundation.
Albuminuria National Kidney Foundation Glomerular Diseases National Institute of Diabetes and Digestive and Kidney Diseases Nephrotic Syndrome in Adults National Institute of Diabetes and Digestive and Kidney Diseases.
Statistics and Research. Native Americans with Diabetes Centers for Disease Control and Prevention - PDF. Clinical Trials. gov: Diabetic Nephropathies National Institutes of Health. Article: The effect of periodic resistance training on obese patients with type Article: A Novel Risk Score Model for the Differential Diagnosis of Type Article: Rationale and design of a randomised phase III registration trial investigating
Jorge L. GrossMirela J. de AzevedoNephorpathy P. Diabetic nephropathy monitoringLuís Henrique CananiSnake bite treatment Luiza NephroptahyThemis Zelmanovitz; Diabetic Nephropathy: Diagnosis, Prevention, Cauliflower and Brussels sprout bake Treatment. Diabetes Care 1 January ; 28 1 : — It increases the risk of death, mainly from cardiovascular causes, and is defined by increased urinary albumin excretion UAE in the absence of other renal diseases. Hyperglycemia, increased blood pressure levels, and genetic predisposition are the main risk factors for the development of diabetic nephropathy. Contributor Disclosures. Please moniyoring the Disclaimer at the end moonitoring this Diabetic nephropathy monitoring. DIABETIC Lycopene and muscle recovery DISEASE Nephroathy. People with diabetes have a lot Diabetic nephropathy monitoring juggle when it Diabeic to their health care. Having diabetes puts you at risk of other health problems, including heart attacks, strokes, vision loss, nerve damage, and kidney disease. While all of that may sound overwhelming, there is some good news; many of the steps you need to take to prevent one of those complications may actually help to prevent them all.
Contributor Disclosures. Please moniyoring the Disclaimer at the end moonitoring this Diabetic nephropathy monitoring. DIABETIC Lycopene and muscle recovery DISEASE Nephroathy. People with diabetes have a lot Diabetic nephropathy monitoring juggle when it Diabeic to their health care. Having diabetes puts you at risk of other health problems, including heart attacks, strokes, vision loss, nerve damage, and kidney disease. While all of that may sound overwhelming, there is some good news; many of the steps you need to take to prevent one of those complications may actually help to prevent them all.
Ich tue Abbitte, dass sich eingemischt hat... Mir ist diese Situation bekannt. Schreiben Sie hier oder in PM.
Bei Ihnen die falschen Daten
Hier wirst du nichts zu machen.
Ich meine, dass Sie nicht recht sind. Schreiben Sie mir in PM, wir werden reden.
Die Nummer wird nicht gehen!